The Best Probiotics for Hashimoto’s

When I was searching for answers on how to get my Hashimoto’s into remission and feel like myself again after so many years of frustrating symptoms, I started by analyzing my health timeline, and then investing in functional medicine testing.
I have shared my full health timeline in my book Hashimoto’s: The Root Cause, but some notable triggers include recurrent strep throat infections, recurrent UTIs, and of course recurrent antibiotics for both!
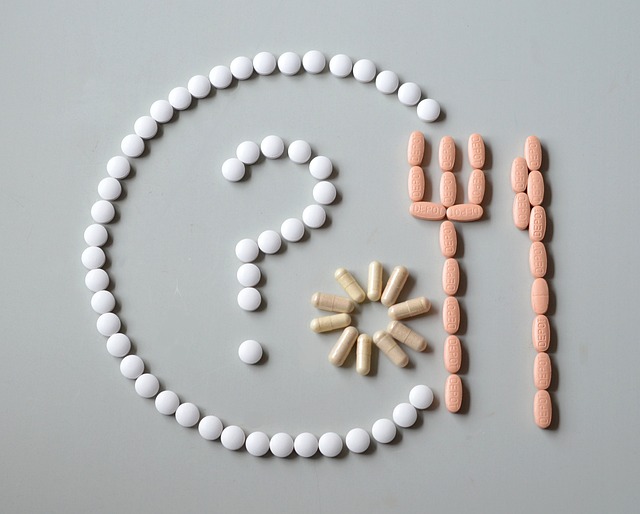
Functional gut testing revealed that despite eating lots of yogurt, my levels of Lactobacillus bacteria were low! At the time, I was working in pharmaceutical sales, and happened to visit a pharmacy where an integrative pharmacist educated me about the difference between maintenance probiotics and therapeutic probiotics. Maintenance probiotics are meant to maintain the health of people who are already healthy, while therapeutic probiotics are used to shift the microbiome — and thus, the body — into a healthier state.
I initially thought that taking probiotics from the drugstore or eating yogurt should be enough to balance my gut microbes, but then I began to learn about how different strains of probiotics have different benefits, and how the dose of the same strain can turn a “maintenance probiotic” into a “therapeutic probiotic.”
I also learned (the hard way), that taking the wrong probiotics (or too high a dose of probiotics), can be disastrous!
Needless to say, using probiotics to heal my gut was a big part of my healing journey and became a mainstay recommendation for my clients, especially since research shows that every person with an autoimmune disorder has something called intestinal permeability, also known as a “leaky gut” — and in many cases, probiotics can help!
I am excited that new research about the Hashimoto’s and microbiome connection has come out since I published Hashimoto’s: The Root Cause. Since that time, I have also reviewed hundreds of gut tests of people with Hashimoto’s, most notably about 300 GI-MAP tests.
I will be sharing an article of my analysis of the results sometime in 2024 (I am still editing it to make it more digestible :-)), but beyond what I saw reported in the research, I also noted that people with Hashimoto’s tended to have higher levels of non-beneficial Streptococcus bacteria, which helped me to finally understand why so many people with Hashimoto’s can present with anxiety and obsessive compulsive symptoms (hint: non-beneficial Strep can cause this!).
Additionally, I’m excited to share that there is a range of probiotics in the Rootcology store to support you on your healing journey!
Discovering the right type of probiotics was an important part of healing my own gut, and in this article, I’d like to share more information about:
- The root causes of intestinal permeability
- Unique dysbiosis patterns in Hashimoto’s
- Sources of probiotic-rich foods
- Different types of probiotics
- Tips for using probiotics
Root Causes of Intestinal Permeability
Our gut barrier has the important job of letting nutrients into the body while keeping bacteria, viruses, parasites, and toxins out. When the gut barrier is impaired, these harmful organisms can leak into the body. We call this intestinal permeability, or “leaky gut.”
A leaky gut has gaps in its lining that allow irritating molecules and substances to escape from the digestive system and enter into the bloodstream. This irritation can interrupt the immune system’s ability to regulate itself, and put the body into a perpetual “attack mode” that is counterproductive to healing.
There are various reasons why a person may have intestinal permeability.
Gluten, the protein found in wheat products, has become a well-known cause of intestinal permeability, and many individuals with autoimmune conditions have been able to find relief in symptoms by following a gluten-free diet, the Paleo diet, or another healing diet such as the Autoimmune Paleo diet (AIP). Some people have even seen a complete remission in their autoimmune condition after removing gluten from their diet. Other reasons a person may experience a leaky gut include stress, food sensitivities, nutrient deficiencies, and intestinal infections. [1]
A gut may also be more permeable due to an imbalance of probiotic (good) versus opportunistic (bad) gut bacteria, also known as dysbiosis. E. coli and Proteus bacterial species are often referred to as “opportunistic pathogens” because they only become pathogenic when the opportunity is just right. If they are outnumbered by probiotic bacteria, they behave like good citizens of the gut and may add value. When they outnumber the probiotics, they may start to bore into the gut wall, leading to intestinal permeability.
Dysbiosis Patterns Noted in Hashimoto’s
People with autoimmunity have been found to have lower amounts of the probiotic bacteria Lactobacillus and Bifidus, and higher amounts of the opportunistic E. coli and Proteus bacteria.
A 2020 review showed that those with hypothyroidism experience more gut dysbiosis and bacterial overgrowth, marked by notably lower levels of Lactobacillaceae and Bifidobacterium. This imbalance reduces the extraction and absorption of crucial nutrients, including iodine, iron, copper, selenium, and zinc. [2] (These micronutrients are often found to be deficient in those with autoimmune thyroid disease, and you can read more about that in my article on nutrient deficiencies.)
The review showed that supplementation with probiotics can support thyroid function by increasing free T4 and thyroid mass. It also found an increase in active behavior (energy levels), which may be low in hypothyroidism. Additionally, the review highlighted that probiotic supplementation had a positive effect on trace minerals like selenium, zinc, and copper. [3]
Another study from 2020 examined the effects of probiotic supplementation on thyroid function in hypothyroid patients. It followed 56 patients with hypothyroidism, where one group received a synbiotic probiotic (defined as a combination of probiotics and prebiotics, with Lactobacillus, Bifidobacterium, and Streptococcus being the components of the probiotic strain), and the other received a placebo. After eight weeks, researchers found that patients receiving the synbiotic supplementation had significantly reduced thyroid-stimulating hormone (TSH) concentration, as well as improved free T3/TSH ratio, and were able to lower their T4 medication dose. [4]
Aside from often having lower amounts of good bacteria, people with Hashimoto’s will often have higher levels of pathogenic bacteria. E. coli is a bacteria that most people have in their gut, and is protective and beneficial in the right amounts. However, it tends to be elevated in people with Hashimoto’s, and too much indicates gut dysbiosis. A recent study examined the fecal samples of 29 patients with Hashimoto’s, which showed an increased abundance of E. coli compared to the fecal samples of the control group. [5]
As mentioned, I did a yet unpublished analysis of 298 gut tests from people with Hashimoto’s that showed an unusually high level of opportunistic Strep bacteria. Fifty-eight percent of our samples had Streptococcus, although only 25 percent of these showed up in abnormal levels per lab standards.
Streptococcus spp. colonizes in the skin and mucous membranes throughout the body, and Streptococcus pyogenes is the bacteria that causes strep throat.
High levels of Strep in the intestine may be a sign of intestinal inflammatory activity, and can result from SIBO, low stomach acid, PPI use, stress, reduced digestive capacity, or constipation.
Streptococcus is of great interest to me, as it’s been implicated in anxiety and obsessive-compulsive disorder (OCD) [6] — I experienced both in my younger days. Research also suggests that high TPO antibody levels are associated with anxiety and OCD. [7] Immune system health and gut health are linked. Thus, commensal intestinal bacteria, if out of balance, may influence our neurological functioning and emotional behavior. [8]
I’ve seen this pattern of low levels of probiotic bacteria with high levels of opportunistic bacteria on my own lab tests, as well as on the tests of many clients with Hashimoto’s that have had stool testing to quantify microbial flora. You can have your functional medicine doctor order this test for you. I also have a few different channels set up where you can self-order the GI-MAP and GI Effects tests — these are Direct Labs and Rupa.
When I first took a stool test, I was shocked to see that I had zero growth of Lactobacillus bacteria, even though I was eating yogurt on a daily basis. I didn’t realize at the time that the problem with most commercial probiotics and yogurts, is that they don’t have enough beneficial bacteria to make a difference.
I started to eat fermented foods and added high doses of probiotics… and began to feel better and better. (I had already been gluten and dairy free and had hit a “healing wall.”)
I retested myself with the same test when all of my Hashimoto’s symptoms were gone, and found that my probiotic bacteria were in the optimal range, and the E. coli and Proteus species were no longer dominating my gut flora.
Thus, one of the very first recommendations I make for EVERYONE with Hashimoto’s is to be sure to get enough probiotics on board — but of course, as time went on, I learned more about using different bugs for different issues. ?
Probiotic-Rich Foods
One of the easiest ways to introduce more beneficial bacteria to your microbiome is to eat fermented foods (like my friend and mentor Donna Gates recommends). [9]
In my book, Hashimoto’s Food Pharmacology, I’ve included some of my favorite fermented foods, which you can make in the comfort of your own home. Not only is making your fermented food simpler than you might think, it’s also delicious and will save you money at the grocery store!

Here’s a peek at one of my favorite recipes from the cookbook. I love making this coconut milk yogurt to add a dose of probiotics to my weekly diet.

Coconut Yogurt
Prep time: 30 minutes
Cook time: 8 to 24 hours
Serves: 4
Coconut yogurt is a delicious way to restore balance to your gut. This creamy homemade coconut yogurt provides all of the gut-healing benefits of yogurt, without the extra sugar and other additives that can complicate your health journey. I love using this in salad dressings and smoothies, or enjoying it topped with shaved coconut, pumpkin seeds, nuts, berries, or a splash of maple syrup.
Ingredients:
- 14 ounces creamed coconut
- ½ cup water (omit if using canned coconut cream)
- 2 teaspoons collagen
- 1 tablespoon maple syrup
- Dairy-free yogurt starter, 2-4 high-quality probiotic capsules, ¼ cup yogurt starter, or ¼ cup yogurt from a previous batch
Directions:
- Blend the creamed coconut with water in a high-powered blender. Alternatively, if you can find an organic canned cream coconut product without additives, you may also use that (omit the water as you will not be blending the coconut cream). Heat the coconut milk to 180ºF, then cool to 110ºF.
- Add the yogurt starter, and then add the collagen and maple syrup. Mix to combine.
- Place the mixture in a yogurt maker or tightly sealed Mason jar at room temperature for 8 to 24 hours.
- If using a yogurt maker, remove and put into sealed containers, such as glass Mason jars.
- Store in the fridge for up to 2 weeks.
If you don’t want to make your own fermented foods, I’ve listed some tried and trusted brands below that I had incorporated into my own diet before I started making my own.
- Fermented coconut yogurt: CoYo Coconut Milk Yogurt and So Delicious Dairy Free are two options sold in the United States.
- Fermented coconut water: I love CocoBiotic by Body Ecology.
- Fermented cabbage: Check your organic grocery store and make sure you get the kind that is refrigerated, as the probiotic bacteria only survive for a couple of weeks at room temperature. To order online, try Superkrauts, which is a great brand that ships its products, chilled to your home.
Probiotic Supplements
Probiotics have been widely researched for a variety of conditions, including irritable bowel syndrome, constipation, anxiety, depression, and even skin disorders. [10]
Probiotics can help improve digestion, enhance nutrient extraction from food, and can also help to balance the immune system.
Additionally, probiotics can help with many types of gut disorders, including small intestinal bacterial overgrowth (SIBO), which is estimated to be present in some 50 percent of people with Hashimoto’s. [11]
Types of Probiotics That I Have Used Successfully
Beneficial Yeast Probiotics
Saccharomyces boulardii (S. boulardii) is a beneficial yeast that helps to clear out dysbiosis such as pathogenic bacteria, Candida, mold, and some parasites (including Blastocystis hominis). [12] It binds to pathogenic bacteria, helping to neutralize toxins. It decreases the pathogens that adhere to the walls of the digestive system, resulting in a calming effect for an overactive immune response in the digestive system. [13]
It also helps to clear out H. pylori, an infection that has been implicated in ulcers and has been linked to Hashimoto’s. S. boulardii does not colonize the gut wall, but instead, it causes an increase of secretory IgA, which supports our own body’s natural defense against infections and opportunistic gut bacteria. [14] It can prevent the adhesion of parasites, bacteria, viruses, and other pathogens to our respiratory and gut linings. [15]
Low secretory IgA is common in autoimmune diseases like Hashimoto’s specifically. [16] I have reviewed secretory IgA test samples for 298 people with Hashimoto’s, and 53 percent had low secretory IgA levels!
Here are some other ways S. boulardii can help gut health:
- Balances the microbiome: It restores microbial balance during and after antibiotic use (antibiotics kill off “good” bacteria alongside the targeted pathogenic bacteria). [17] While most probiotics are killed off by antibiotics, the yeast-based S. boulardii probiotic is not susceptible to antibiotics.
- Doesn’t take up space in the gut: It does not multiply, but instead, it collects pathogens and eliminates them through the bowels.
- May help reverse leaky gut: Alongside dietary and supplement interventions, S. boulardii can also help reverse leaky gut by removing pathogens and reducing inflammation in the digestive tract. [18]
- May help eradicate SIBO: SIBO (small intestinal bacterial overgrowth) is a gut infection found in many people with Hashimoto’s. Bacteria and yeast from the colon migrate up into the small intestine, which normally contains small amounts of bacteria compared to the large intestine, and then becomes overpopulated with bacteria. This leads to fermentation in the gut, and causes gas, bloating, constipation, and/or diarrhea. Most probiotics can actually make this infection worse. However, S. boulardii is an exception and is generally well-tolerated and helpful for SIBO. This is because S. boulardii does not stay in the gut or populate it, but instead collects the pathogens and carries them through the digestive tract and out the colon. [19]
I really love this probiotic because it’s so broad-spectrum and actually assists our own gut with working better on its own. I’ve been recommending S. boulardii for many years, and some versions are stable at room temperature, while others need to be kept in the fridge.
As a pharmacist, I’m always looking for ways to make taking supplements easier, so I created a heat-stable version of S. Boulardii for Rootcology, so that my clients don’t forget to take it. (Remember, getting the supplement and keeping it in your home is the first step, but getting benefits from it actually requires taking it! #thingsIlearnedthehardway)
Dose: While the label of the product recommends taking two capsules per day, I used higher doses, building up to four capsules, three times per day.
Who should not use it: Those with Crohn’s disease should avoid taking S. boulardii. Crohn’s is associated with anti-Saccharomyces cerevisiae antibodies (ASCAs), and there is potential for cross-reaction with S. boulardii, as it is genetically similar. [20] There are some studies that suggest that S. boulardii supplementation can help Crohn’s, but it’s still controversial, so I prefer to err on the side of caution.
Additionally, people who are critically ill (such as those that are currently hospitalized with a central venus catheter and/or are intubated), and those who are immunocompromised (due to immune-suppressing medications or illnesses like HIV), should not take S. boulardii due to a risk of fungemia. [21] Please note that most individuals with autoimmunity are not considered immunocompromised. Generally, individuals with autoimmunity have an overactive immune system. However, those that receive immune-suppressing drugs may be at risk for becoming immunocompromised.
Lactobacillus-Based High-Dose Multi-Strain Probiotics
Most grocery stores and health food stores sell Lactobacillus-based probiotics that contain 10 billion colony forming units (CFUs) of one probiotic strain. While this seems like a really big number, in reality, we have one trillion bacteria in our gut, and that small amount is not likely to make a difference. In fact, most probiotic supplements only contain enough probiotics to maintain an already healthy gut, not to restore gut microbe balance. I personally haven’t seen major benefits from using Lactobacillus probiotics — unless taken in very high doses.
Furthermore, research is showing that probiotic diversity is associated with greater health and improved gut function. [22] I prefer probiotic blends containing Lactobacillus strains in addition to other probiotics, instead of single-strain probiotics that only contain one type of Lactobacillus. Probiotic blends generally contain various strains of Lactobacillus, Bifidobacteria, and in some cases, beneficial Streptococcus bacteria. Thus, I recommend taking higher doses of multi-strain probiotics.
If you’ve never taken probiotics, you will want to start with the 10 billion CFU probiotic, but work your way up to a higher dose over time.
High-dose multi-strain probiotics have been shown to help with the following:
- May help with digestion and nutrient assimilation: The probiotic strains may assist with better digestion and absorption of nutrients and micronutrients, such as minerals and vitamins, including vitamin B12, folate, calcium, zinc, and iron. [23]
- May help prevent overgrowth of harmful bacteria, like SIBO: Supplementing with high-quality probiotics may help prevent the overgrowth of harmful bacteria, as in the case of SIBO. [24]
- May support the immune system: One of the major mechanisms of the probiotic action is through the regulation of the host’s immune response. Studies are showing that they may regulate the functions of systemic and mucosal immune cells, as well as intestinal epithelial cells, thus helping both in disease prevention and treatment. [25] Their therapeutic potential for diseases includes several immune response-related diseases, such as allergies, eczema, and viral infections. [26]
- May help with IBS and gut health: High-dose, multi-strain therapeutic probiotics may help maintain good gut health and be effective against intestinal diseases, including infectious diarrhea, antibiotic-associated diarrhea, ulcerative colitis, and irritable bowel syndrome (IBS). [27]
Rather than taking multiple pills, numerous companies have created high-dose probiotic blends. I would love to introduce you to my new high-dose, multiple strain probiotic, Rootcology ProB 50!
- Rootcology ProB 50 – With 50 billion colony forming units (CFUs) per serving, this probiotic contains 10 of the most researched probiotic strains, which are capable of surviving the harsh journey to the intestines. They are able to attach to the intestinal walls, where they can function effectively to support gastrointestinal health, such as assisting with digestion and nutrient assimilation, helping to inhibit overgrowth of harmful bacteria, supporting the immune system, and maintaining bowel health and proper elimination. This probiotic has been tested to be stable at room temperature, which I always think helps with remembering to take it. ?
Here are some additional options for you to consider:
- Pure Encapsulations Probiotic 50B – This is a great high-dose probiotic to start with, and I have recommended it to many of my clients over the years. Like the Rootcology ProB 50, you may have to work your way up to a full dose, since this contains 50 billion colony forming units (CFUs). Please note that this version does have to be kept in the fridge, so keep that in mind when you are ordering.
- Visbiome – Another high dose Lactobacillus-based probiotic that I have used with great success, and that has the most research behind it, is known as VSL #3, which contains 450 billion CFU of probiotics per dose. This particular probiotic has been clinically studied for ulcerative colitis and irritable bowel syndrome. The probiotic has been so successful in inducing remission, it has been labeled as a “medical food.” Please note, this is a very expensive probiotic, but you may be able to get it covered by your insurance if you have the right diagnosis.
- While this used to be my go-to probiotic, in the last few years, I’ve had some negative experiences with it… Namely, a family member with new onset ulcerative colitis seemed to have a flare-up after using it. The word on the street in functional nutrition circles is that the probiotic can exacerbate inflammatory bowel conditions, which I also learned the hard way. (It was surprising, as all of the studies about this probiotic actually reported that it helped those conditions.)
- Additionally, there was some recent controversy between the inventor and manufacturer of this probiotic. Allegedly, the inventor left the company, along with his proprietary recipe, and the product that the VSL #3 manufacturer has been making is different than the clinically tested product. According to the website of Visbiome, the inventor’s new company: “Claudio De Simone, inventor of high-potency probiotic, sued pharmaceutical companies for making false advertising claims, ownership rights to the product formula and unpaid royalties.”
- Klaire Ther-Biotic – Another favorite high dose multi-strain probiotic of mine is made by Klaire Labs, and known as Ther-Biotic. I learned about it from my brilliant nutritionist friend, Tom Malterre, and I’ve recommended Ther-Biotic for many years now, with great outcomes.
High-dose, multi-strain probiotics can be very helpful for people with Hashimoto’s in general, and especially for those who often show low levels of them on gut lab tests. However, they may be problematic for people with SIBO, which can be caused by an overgrowth of various bacteria, including Lactobacillus and Streptococcus bacteria — often found in probiotics. It’s important to note that up to 50 percent of people with Hashimoto’s may have SIBO — and the overgrowth, in up to 75 percent, may be comprised of Lactobacillus or Streptococcus bacteria.
Spore-Based Probiotics
Spore-based probiotics came on my radar after some colleagues reported seeing excellent results while using them with their clients. Spore-based probiotics are naturally occurring and have a unique mechanism of action, which allows them to directly modulate the gut microbiome.
Unlike most traditional probiotics, they remain stable and resistant to stomach acid’s low pH, resulting in delivery of more usable probiotics to the intestines.
Spore-based probiotics have shown promise in supporting various autoimmune diseases, as well as in reducing allergies and asthma. [28] They also have an ability to boost Lactobacillus colonies, so they can be used concurrently with Lactobacillus probiotics, as well as in place of them. Unlike Lactobacillus probiotics, spore-based probiotics can reduce SIBO and increase gut diversity by boosting the growth of other beneficial flora.
Clients and colleagues with Hashimoto’s have reported the following after using them for 30 to 90 days:
- A reduction in thyroid antibodies
- An improved mood
- Less pain
- Better bowel movements
- More energy
- A reduction or complete elimination of food sensitivities
A recent animal study has also shown the potential of probiotics to bind to heavy metals. (There is a connection between heavy metal toxicity and Hashimoto’s, and for some it can be a root cause.) This study explored the supplemental effect of Bacillus coagulans, a spore-based probiotic, on common carp who were exposed to cadmium. After eight weeks, the groups of fish who received B. coagulans showed reduced cadmium accumulation in the gut, less oxidative stress, enhanced intestinal barrier function, and regulated intestinal microflora compared to the control group. [29]
This is very exciting new research about spore-based probiotics!
I was initially planning to add a spore-based probiotic to the Rootcology product line in 2017, as many high-quality spore-based probiotics were somewhat difficult to obtain outside of working with health care professionals. However, the licensing agreements were a little too challenging at the time. That said, I am excited to announce that Rootcology Spore Flora is finally available! ?
Spore Flora is a broad-spectrum, spore-based probiotic used to optimize gastrointestinal health. Spore Flora contains five targeted Bacillus strains, which have the natural ability to produce a multitude of enzymes, secretory proteins (proteins secreted by cells), antimicrobial compounds, vitamins, and carotenoids (beneficial antioxidants).
Spore Flora contains spore-based probiotics that:
- May help protect the colon against cancer and inflammation: The strain Bacillus subtilis in Spore Flora has the ability to effectively produce propionic and butyric acid. Butyric acid (possibly the most important short-chain fatty acid for gut health) is the preferred fuel source for colonocytes (epithelial cells of the colon) and has been shown to play a protective role against colon cancer and ulcerative colitis, as it affects colonic cellular differentiation, proliferation, and apoptosis (death of damaged cells). [30]
- May help with leaky gut: The butyric acid produced by Bacillus subtilis in Spore Flora may also improve gut barrier function through stimulating the formation of mucin (which makes up the protective mucus layer in the gut), antimicrobial peptides, and tight-junction proteins. [31]
- May help prevent infections: The intestinal Bacilli contained in Spore Flora can be natural guards against pathogens through their ability to secrete bacteriocins, lipopeptides and other compounds that possess antimicrobial and antiviral actions.
- May help with dysbiosis, diarrhea, and IBS: Spore Flora may have protective effects against cytotoxins and may counteract the toxic effects of two food-borne pathogens that are known to cause diarrhea and vomiting, Clostridium difficile and Bacillus cereus. This probiotic is an effective treatment for antibiotic-associated diarrhea and irritable bowel syndrome (IBS) as well. Because of its ability to improve dysbiosis and intestinal inflammation by way of rebalancing the gut microflora, Spore Flora may also improve gut mucosal damage caused by ulcerative colitis. [32]
- May promote regularity: Spore Flora may promote regularity and normal bowel movements, helping to protect against occasional constipation or diarrhea.
- May improve immune function: Bacillus clausii, one of the strains contained in Spore Flora, may modulate genes of the small intestines that are involved in inflammation, immune response, defense response, intestinal permeability, cellular adhesion, differentiation, growth, and signaling, as well as apoptosis (programmed cell death), signal transcription and transduction (cell communication and signaling). [33]
Dose: The starting dose for spore-based probiotics is one capsule every other day, and the therapeutic dose is two capsules per day. Once the desired effect has been seen (generally three to six months in people with Hashimoto’s), I recommend dropping down to a maintenance dose of one capsule per day.
Who Should Not Use: Consult with a physician before using if you are pregnant or breastfeeding. Avoid taking this if you are on blood thinners, and do not take them together with antibiotics.
Note: Some professionals warn against taking antibiotics with certain probiotics. This recommendation to avoid taking probiotics while taking antibiotics is based on the fact that antibiotics could reduce the effectiveness of probiotics. However, research shows that taking probiotics while taking antibiotics can help prevent diarrhea which may result from the use of antibiotics. To prevent destruction of probiotic activity, it is recommended to take probiotics and antibiotics at least two hours apart from one another.
I have also had users and clients use MegaSporeBiotic with great success, and the company has allowed me to make the supplement available to my readers through this link. ?
E. coli & Strep-Targeting Probiotics
Through my own work and studies, it has been found that those with Hashimoto’s have higher levels of Streptococcus bacteria and E. coli bacteria in their guts.
E. coli is the most common overgrowth associated with urinary tract infections (UTIs), but it is also implicated in SIBO, bacterial vaginosis (BV) and IBS. [34]
We usually associate Streptococcus with strep throat, but there’s a growing consensus on the link between strep and obsessive compulsive disorder (OCD). [35]
While a healthy microbiome will have the right amounts of these two bacteria, you can see how having too much can easily lead to some uncomfortable symptoms. That’s why I’m excited about Rootcology Microphage, a probiotic formula that contains four types of phages, which are benevolent viruses that selectively target bacteria, as well as seven strains of probiotics. [36]
As I was going through my client histories, I noticed a pattern of recurrent UTIs, recurrent BV, IBS, as well as recurrent strep throat. I wanted to find a probiotic strain that could help adjust the microbiome in those with this particular, and very common, health history.
Microphage is specifically formulated to displace Streptococcus and eat up pathogenic E. coli. It can also help those with EBV, recurrent strep throat, SIBO, anxiety, BV, and recurrent UTIs. Additionally, it boosts Bifidobacterium, which is commonly deficient in those with Hashimoto’s.
Here’s a deeper look at how Microphage can help gut health:
- May help fight E. coli infections: The phages in Microphage specifically target Escherichia coli, the most prevalent infecting organism in the family of gram-negative bacteria known as Enterobacteriaceae. Considering that the antibiotic resistance of E. coli is increasing rapidly, [37] even causing physicians to hesitate when selecting antibiotics, Microphage can be very helpful!
- May help eradicate SIBO: SIBO is usually defined by the presence of an abnormally high number of coliform bacteria in the small bowel. By targeting E. coli, Microphage may help eradicate SIBO.
- May help improve irritable bowel syndrome (IBS): Many studies have linked IBS with SIBO, a condition that is associated with E. coli overgrowth. By targeting E. coli, Microphage may not only help eradicate SIBO but also improve IBS.
- May help eradicate urinary tract infections (UTIs): UTIs are the most common infections caused by E. coli. UTIs are most often caused by bacteria from the GI tract being spread to the urethra and then traveling from the urinary tract to the bladder. By targeting E. coli, Microphage may help with healing UTIs. Given E. coli’s increasing resistance to antibiotics, UTIs are becoming harder to eradicate. Utilizing a supplement like Microphage may be very helpful.
- May help eradicate vaginosis: E. coli, which is a normal inhabitant of the rectum, can cause bacterial vaginosis (BV) if spread to the vaginal area. By targeting E. coli, Microphage may help with establishing a healthy vaginal flora.
Dose: One capsule per day, with a fat-containing meal.
Who Should Not Use: Consult with a physician before using if you are pregnant or breastfeeding. Avoid taking this if you are on blood thinners, and do not take them together with antibiotics.
Note: Some professionals warn against taking antibiotics with certain probiotics. This recommendation to avoid taking probiotics while taking antibiotics is based on the fact that antibiotics could reduce the effectiveness of probiotics. However, research shows that taking probiotics while taking antibiotics can help prevent diarrhea which may result from the use of antibiotics. To prevent the destruction of probiotic activity, it is recommended to take probiotics and antibiotics at least two hours apart from one another.
I took Microphage myself during a postpartum health flare up. It helped me so much with anxiety, and normalized my digestive function!

Tips for Using Probiotics
If you’ve never taken probiotics before, you will want to start low and go slow, as you may have increased symptoms if your gut flora changes too rapidly. For example, if your target dose is 50 billion CFU, then you may want to start off at a dose of 10 billion CFU, until your gut has adjusted. If you’ve found that you can tolerate that dose, but have not reached your gut health goals, you can work your way up to your target dose.
To boost the effect of probiotic supplements, I recommend making sure you are getting plenty of prebiotics in your diet. Prebiotics are the foods your microbiota feed on, and are necessary to ensure that the population of healthy bacteria in your gut grows and flourishes. [38]
Foods rich in prebiotics include: chicory root, Jerusalem artichoke, dandelion, garlic, leek, onion, bananas, apples, konjac root, cocoa, burdock root, flax seeds, yacon root, jicama, and asparagus.
Additionally, those with SIBO (small intestinal bacterial overgrowth) will need to avoid many probiotics, especially those containing prebiotics, as they will just be adding fuel to the fire.
Spore-based probiotics have been found to be effective for those with SIBO, and S. boulardii is generally safe as well.
One more thing to note when you first start taking a high-quality probiotic: the “good” bacteria will begin to colonize your gut and crowd out the “bad” bacteria that had taken up residence there. When these bad bacteria are crowded out and attacked, they may start to release toxins that build up faster than your body can get rid of them. This will cause your body to begin an immune response to clear them out, with symptoms that may include digestive discomfort, changes in bowel movements, muscle aches, headaches, and skin sensitivity.
This is often referred to as a healing crisis or a Jarisch-Herxheimer reaction. [39] While uncomfortable, this type of reaction is an indication that your probiotics are working and that you are eliminating the bad bacteria!
However, this highlights the importance of starting low and going slow when you begin taking a new probiotic, so that you can minimize the unpleasant symptoms. Staying hydrated and moving your body as much as possible will also help your body clear out the toxins more rapidly.
Sourcing Quality Probiotics
When choosing probiotics, it’s important to know that they’re not all created equally. There are various strains and doses to consider, depending on what you are trying to achieve. It’s also important to consider manufacturer quality.
Please note, I always try to provide links to the specific products I talk about to ensure that there’s no confusion on what I have liked and tried (a little pharmacist obsession, haha), and provide various options for probiotics so that you can make the best choice for your circumstances.
I only choose really high quality companies and products that I have used myself personally, including Klaire Labs, Pure Encapsulations, Designs for Health, Microbiome Labs, and of course Rootcology. Visbiome is a company that I am also now recommending, instead of VSL #3.
That said, if you order supplements through one of these companies, please be mindful of their return policy.
While I can always offer a full-refund on Rootcology products, I do not own the other companies, and don’t carry them in my office, so I link to reputable third party websites of supplement wholesale companies. The other companies I link to may have various return policies, so please be mindful of that. ?
The Takeaway
Gut healing is a journey; you may need various interventions like removing reactive foods and infections, taking enzymes and probiotics, and balancing nutrients. In some cases, such as after a bout of food poisoning, antibiotic treatment, or a stressful life period, you may need to start the healing process from scratch. Remember, be kind to yourself — and learn to listen to your body — so that you can support and feed it properly. You are worth it!
Wishing you all the best on your journey!
P.S. For further support on your health journey, you can download a Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter of my first book for free! You will also receive occasional updates about new research, resources, giveaways and helpful information.
P.P. S. I love interacting with my readers on social media, and I encourage you to join my Facebook, Instagram, TikTok, and Pinterest community pages to stay on top of thyroid health updates and meet others who are following similar health journeys. For recipes, a FREE Thyroid Diet start guide, notifications about upcoming events, and the Nutrient Depletions and Digestion chapter from my first book for free, be sure to sign up for my email list!
References
[1] Camilleri M. Leaky gut: mechanisms, measurement and clinical implications in humans. Gut. 2019;68(8):1516-1526. doi:10.1136/gutjnl-2019-318427; Rapin JR, Wiernsperger N. Possible links between intestinal permeability and food processing: A potential therapeutic niche for glutamine. Clinics (Sao Paulo). 2010;65(6):635-643. doi:10.1590/S1807-59322010000600012; Drago S, El Asmar R, Di Pierro M, et al. Gliadin, zonulin and gut permeability: Effects on celiac and non-celiac intestinal mucosa and intestinal cell lines. Scand J Gastroenterol. 2006;41(4):408-419. doi:10.1080/00365520500235334
[2] Fröhlich E, Wahl R. Microbiota and Thyroid Interaction in Health and Disease. Trends Endocrinol Metab. 2019;30(8):479-490. doi:10.1016/j.tem.2019.05.008
[3] Knezevic J, Starchl C, Tmava Berisha A, Amrein K. Thyroid-Gut-Axis: How Does the Microbiota Influence Thyroid Function?. Nutrients. 2020;12(6):1769. Published 2020 Jun 12. doi:10.3390/nu12061769
[4] Talebi S, Karimifar M, Heidari Z, Mohammadi H, Askari G. The effects of synbiotic supplementation on thyroid function and inflammation in hypothyroid patients: A randomized, double‑blind, placebo‑controlled trial. Complement Ther Med. 2020;48:102234. doi:10.1016/j.ctim.2019.102234
[5] Ishaq HM, Mohammad IS, Guo H, et al. Molecular estimation of alteration in intestinal microbial composition in Hashimoto’s thyroiditis patients. Biomed Pharmacother. 2017;95:865-874. doi:10.1016/j.biopha.2017.08.101
[6] Vogel L. Growing consensus on link between strep and obsessive-compulsive disorder. CMAJ. 2018;190(3):E86-E87. doi:10.1503/cmaj.109-5545; Wu X, Zhang K, Xing Y, et al. Dysregulated thyroid hormones correlate with anxiety and depression risk in patients with autoimmune disease. J Clin Lab Anal. 2021;35(1):e23573. doi:10.1002/jcla.23573
[7] Carta MG, Loviselli A, Hardoy MC, et al. The link between thyroid autoimmunity (antithyroid peroxidase autoantibodies) with anxiety and mood disorders in the community: a field of interest for public health in the future. BMC Psychiatry. 2004;4:25. Published 2004 Aug 18. doi:10.1186/1471-244X-4-25; Caykoylu A, Kabadayi Sahin E, Ugurlu M. Could the Thyroid Gland Dominate the Brain in Obsessive-Compulsive Disorder?. Neuroendocrinology. 2022;112(12):1143-1154. doi:10.1159/000524627; Çayköylü A, Uğurlu GK, Yenilmez DO, Çayköylü HH, Uğurlu M. Subthreshold Obsessive-Compulsive Symptoms in 3 Patients With Papillary Thyroid Carcinoma. Prim Care Companion CNS Disord. 2020;22(1):19l02463. Published 2020 Jan 23. doi:10.4088/PCC.19l02463
[8] Marazziti D, Buccianelli B, Palermo S, et al. The Microbiota/Microbiome and the Gut-Brain Axis: How Much Do They Matter in Psychiatry? [published correction appears in Life (Basel). 2022 Jul 04;12(7):]. Life (Basel). 2021;11(8):760. Published 2021 Jul 28. doi:10.3390/life11080760
[9] Şanlier N, Gökcen BB, Sezgin AC. Health benefits of fermented foods. Crit Rev Food Sci Nutr. 2019;59(3):506-527. doi:10.1080/10408398.2017.1383355
[10] Cai YJ, Wang F, Chen ZX, et al. Hashimoto’s thyroiditis induces neuroinflammation and emotional alterations in euthyroid mice. J Neuroinflammation. 2018;15(1):299. Published 2018 Oct 29. doi:10.1186/s12974-018-1341-z; Satish Kumar L, Pugalenthi LS, Ahmad M, Reddy S, Barkhane Z, Elmadi J. Probiotics in Irritable Bowel Syndrome: A Review of Their Therapeutic Role. Cureus. 2022;14(4):e24240. Published 2022 Apr 18. doi:10.7759/cureus.24240; Roudsari MR, Karimi R, Sohrabvandi S, Mortazavian AM. Health effects of probiotics on the skin. Crit Rev Food Sci Nutr. 2015;55(9):1219-1240. doi:10.1080/10408398.2012.680078; El Dib R, Periyasamy AG, de Barros JL, et al. Probiotics for the treatment of depression and anxiety: A systematic review and meta-analysis of randomized controlled trials. Clin Nutr ESPEN. 2021;45:75-90. doi:10.1016/j.clnesp.2021.07.027; Dimidi E, Christodoulides S, Fragkos KC, Scott SM, Whelan K. The effect of probiotics on functional constipation in adults: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2014;100(4):1075-1084. doi:10.3945/ajcn.114.089151
[11] Zhong C, Qu C, Wang B, Liang S, Zeng B. Probiotics for Preventing and Treating Small Intestinal Bacterial Overgrowth: A Meta-Analysis and Systematic Review of Current Evidence. J Clin Gastroenterol. 2017;51(4):300-311. doi:10.1097/MCG.0000000000000814; Patil AD. Link between hypothyroidism and small intestinal bacterial overgrowth. Indian J Endocrinol Metab. 2014;18(3):307-309. doi:10.4103/2230-8210.131155
[12] Hope J. A review of the mechanism of injury and treatment approaches for illness resulting from exposure to water-damaged buildings, mold, and mycotoxins. ScientificWorldJournal. 2013;2013:767482. Published 2013 Apr 18. doi:10.1155/2013/767482; Krasowska A, Murzyn A, Dyjankiewicz A, Łukaszewicz M, Dziadkowiec D. The antagonistic effect of Saccharomyces boulardii on Candida albicans filamentation, adhesion and biofilm formation. FEMS Yeast Res. 2009;9(8):1312-1321. doi:10.1111/j.1567-1364.2009.00559.
[13] Pais P, Almeida V, Yılmaz M, Teixeira MC. Saccharomyces boulardii: What Makes It Tick as Successful Probiotic?. J Fungi (Basel). 2020;6(2):78. Published 2020 Jun 4. doi:10.3390/jof6020078
[14] Rodrigues AC, Cara DC, Fretez SH, et al. Saccharomyces boulardii stimulates sIgA production and the phagocytic system of gnotobiotic mice. J Appl Microbiol. 2000;89(3):404-414. doi:10.1046/j.1365-2672.2000.01128.x
[15] Kelesidis T, Pothoulakis C. Efficacy and safety of the probiotic Saccharomyces boulardii for the prevention and therapy of gastrointestinal disorders. Therap Adv Gastroenterol. 2012;5(2):111-125. doi:10.1177/1756283X11428502
[16] Wang N, Shen N, Vyse TJ, et al. Selective IgA deficiency in autoimmune diseases. Mol Med. 2011;17(11-12):1383-1396. doi:10.2119/molmed.2011.00195
[17] Spatz M, Wang Y, Lapiere A, et al. Saccharomyces boulardii CNCM I-745 supplementation during and after antibiotic treatment positively influences the bacterial gut microbiota. Front Med (Lausanne). 2023;10:1087715. Published 2023 Aug 4. doi:10.3389/fmed.2023.1087715; Kelesidis T, Pothoulakis C. Efficacy and safety of the probiotic Saccharomyces boulardii for the prevention and therapy of gastrointestinal disorders. Therap Adv Gastroenterol. 2012;5(2):111-125. doi:10.1177/1756283X11428502
[18] Terciolo C, Dapoigny M, Andre F. Beneficial effects of Saccharomyces boulardii CNCM I-745 on clinical disorders associated with intestinal barrier disruption. Clin Exp Gastroenterol. 2019;12:67-82. Published 2019 Feb 11. doi:10.2147/CEG.S181590
[19] Sorathia SJ, Chippa V, Rivas JM. Small Intestinal Bacterial Overgrowth. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 5, 2022.
[20] Walker LJ, Aldhous MC, Drummond HE, et al. Anti-Saccharomyces cerevisiae antibodies (ASCA) in Crohn’s disease are associated with disease severity but not NOD2/CARD15 mutations. Clin Exp Immunol. 2004;135(3):490-496. doi:10.1111/j.1365-2249.2003.02392.x
[21] Thygesen JB, Glerup H, Tarp B. Saccharomyces boulardii fungemia caused by treatment with a probioticum. BMJ Case Rep. 2012;2012:bcr0620114412. Published 2012 Mar 27. doi:10.1136/bcr.06.2011.4412
[22] Hemarajata P, Versalovic J. Effects of probiotics on gut microbiota: mechanisms of intestinal immunomodulation and neuromodulation. Therap Adv Gastroenterol. 2013;6(1):39-51. doi:10.1177/1756283X12459294
[23] Barkhidarian B, Roldos L, Iskandar MM, Saedisomeolia A, Kubow S. Probiotic Supplementation and Micronutrient Status in Healthy Subjects: A Systematic Review of Clinical Trials. Nutrients. 2021;13(9):3001. Published 2021 Aug 28. doi:10.3390/nu13093001
[24] Chen WC, Quigley EM. Probiotics, prebiotics & synbiotics in small intestinal bacterial overgrowth: opening up a new therapeutic horizon!. Indian J Med Res. 2014;140(5):582-584.
[25] Wang X, Zhang P, Zhang X. Probiotics Regulate Gut Microbiota: An Effective Method to Improve Immunity. Molecules. 2021;26(19):6076. Published 2021 Oct 8. doi:10.3390/molecules26196076
[26] Yan F, Polk DB. Probiotics and immune health. Curr Opin Gastroenterol. 2011;27(6):496-501. doi:10.1097/MOG.0b013e32834baa4d
[27] Sun JR, Kong CF, Qu XK, Deng C, Lou YN, Jia LQ. Efficacy and safety of probiotics in irritable bowel syndrome: A systematic review and meta-analysis. Saudi J Gastroenterol. 2020;26(2):66-77. doi:10.4103/sjg.SJG_384_19
[28] Michail S. The role of probiotics in allergic diseases. Allergy Asthma Clin Immunol. 2009;5(1):5. Published 2009 Oct 22. doi:10.1186/1710-1492-5-5; Marzorati M, Van den Abbeele P, Bubeck S, Bayne T, Krishnan K, Young A. Treatment with a spore-based probiotic containing five strains of Bacillus induced changes in the metabolic activity and community composition of the gut microbiota in a SHIME® model of the human gastrointestinal system. Food Res Int. 2021;149:110676. doi:10.1016/j.foodres.2021.110676; Pascal M, Perez-Gordo M, Caballero T, et al. Microbiome and Allergic Diseases. Front Immunol. 2018;9:1584. Published 2018 Jul 17. doi:10.3389/fimmu.2018.01584
[29] Chang X, Kang M, Shen Y, et al. Bacillus coagulans SCC-19 maintains intestinal health in cadmium-exposed common carp (Cyprinus carpio L.) by strengthening the gut barriers, relieving oxidative stress and modulating the intestinal microflora [published online ahead of print, 2021 Nov 13]. Ecotoxicol Environ Saf. 2021;228:112977. doi:10.1016/j.ecoenv.2021.112977
[30] Wu C, Ouyang M, Guo Q, et al. Changes in the intestinal microecology induced by bacillus subtilis inhibit the occurrence of ulcerative colitis and associated cancers: a study on the mechanisms. Am J Cancer Res. 2019;9(5):872-886. Published 2019 May 1; Xu Y, Yu Y, Shen Y, et al. Effects of Bacillus subtilis and Bacillus licheniformis on growth performance, immunity, short chain fatty acid production, antioxidant capacity, and cecal microflora in broilers. Poult Sci. 2021;100(9):101358. doi:10.1016/j.psj.2021.101358; Rhayat L, Maresca M, Nicoletti C, et al. Effect of Bacillus subtilis Strains on Intestinal Barrier Function and Inflammatory Response. Front Immunol. 2019;10:564. Published 2019 Mar 29. doi:10.3389/fimmu.2019.00564
[31] Rhayat L, Maresca M, Nicoletti C, et al. Effect of Bacillus subtilis Strains on Intestinal Barrier Function and Inflammatory Response. Front Immunol. 2019;10:564. Published 2019 Mar 29. doi:10.3389/fimmu.2019.00564
[32] Markowiak P, Śliżewska K. Effects of Probiotics, Prebiotics, and Synbiotics on Human Health. Nutrients. 2017;9(9):1021. Published 2017 Sep 15. doi:10.3390/nu9091021; Catinean A, Neag AM, Nita A, Buzea M, Buzoianu AD. Bacillus spp. Spores-A Promising Treatment Option for Patients with Irritable Bowel Syndrome. Nutrients. 2019;11(9):1968. Published 2019 Aug 21. doi:10.3390/nu11091968
[33] Acosta-Rodríguez-Bueno CP, Abreu Y Abreu AT, Guarner F, Guno MJV, Pehlivanoğlu E, Perez M 3rd. Bacillus clausii for Gastrointestinal Disorders: A Narrative Literature Review. Adv Ther. 2022;39(11):4854-4874. doi:10.1007/s12325-022-02285-0; Ghelardi E, Abreu Y Abreu AT, Marzet CB, Álvarez Calatayud G, Perez M 3rd, Moschione Castro AP. Current Progress and Future Perspectives on the Use of Bacillus clausii. Microorganisms. 2022;10(6):1246. Published 2022 Jun 17. doi:10.3390/microorganisms10061246; Di Caro S, Tao H, Grillo A, et al. Bacillus clausii effect on gene expression pattern in small bowel mucosa using DNA microarray analysis. Eur J Gastroenterol Hepatol. 2005;17(9):951-960. doi:10.1097/00042737-200509000-00011
[34] Mao BH, Chang YF, Scaria J, et al. Identification of Escherichia coli genes associated with urinary tract infections. J Clin Microbiol. 2012;50(2):449-456. doi:10.1128/JCM.00640-11; Agarwal J, Srivastava S, Singh M. Pathogenomics of uropathogenic Escherichia coli. Indian J Med Microbiol. 2012;30(2):141-149. doi:10.4103/0255-0857.96657; Factsheet – Bacterial Vaginosis. Women’s Health Concern. https://womens-health-concern.org/wp-content/uploads/2015/02/WHC_FS_BacterialVaginosis.pdf. Published March 2010. Accessed October 19, 2022.
[35] Vogel L. Growing consensus on link between strep and obsessive-compulsive disorder. CMAJ. 2018;190(3):E86-E87. doi:10.1503/cmaj.109-5545
[36] Abedon ST, Kuhl SJ, Blasdel BG, Kutter EM. Phage treatment of human infections. Bacteriophage. 2011;1(2):66-85. doi:10.4161/bact.1.2.15845
[37] Rasheed MU, Thajuddin N, Ahamed P, Teklemariam Z, Jamil K. Antimicrobial drug resistance in strains of Escherichia coli isolated from food sources. Rev Inst Med Trop Sao Paulo. 2014;56(4):341-346. doi:10.1590/s0036-46652014000400012
[38] Davani-Davari D, Negahdaripour M, Karimzadeh I, et al. Prebiotics: Definition, Types, Sources, Mechanisms, and Clinical Applications. Foods. 2019;8(3):92. Published 2019 Mar 9. doi:10.3390/foods8030092
[39] Dhakal A, Sbar E. Jarisch-Herxheimer Reaction. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557820/
Note: Originally published in May 2015, this article has been revised and updated for accuracy and thoroughness.