Depression is a topic near and dear to my heart.
Many moons ago, I lost a loved one to suicide… and while I’ll never understand the immense pain of a person in the moment before they choose to end their life, I can tell you that the loss leaves families and survivors (like me), in utter devastation and despair. Some even spiral into a deep depression from the trauma.
I was one of them.
Losing my loved one created the type of hole in my heart that I hope others never have to experience, and was likely a factor in the development or exacerbation of my autoimmune condition.
I personally battled with depression before my Hashimoto’s diagnosis. I had worked and interned in various mental health settings as a pharmacy student for about 10 years, with the goal of specializing in psychopharmacology, before realizing that I had Hashimoto’s — and that perhaps there was more to treating mood disorders than a prescription pad.
In my experience with my thyroid clients with depression, we’ve had about an 80 percent success rate using the very strategies I share below.
For the last decade, depression has become a distant memory for me. On most days, I feel calm, happy, and empowered, and sometimes forget how it feels to not be in a great mood every day.
The past few years have been so hard on many of us, including me, and I wanted to share this article with you, with the hope that it will offer you some new information to help you cope if you are struggling with depression. I’ve noticed that since 2020, many of us need to do EXTRA to support our mental health.
I share this information with you, and I hope that you will benefit from it and also share it with someone you care about who may need it. How I wish I knew then what I know now. It breaks my heart that some of the kindest and most amazing people I used to know are no longer around to enjoy the beauty of this world, and that others are not living their lives due to the dark cloud of depression hovering over their heads.
If you’re reading this, please know this: often depression can be resolved when an underlying thyroid issue is addressed.
While there are reasons for depression beyond thyroid health, because it’s Thyroid Awareness Month, and because I am the Thyroid Pharmacist, I would love to share the connection between thyroid issues and depression in my little corner of the internet.
Some people struggle for years without a proper diagnosis of thyroid disease — and even worse, many of those with a proper thyroid diagnosis don’t receive the right treatment and continue to have depression. It breaks my heart to think about the many thyroid patients who get labeled as clinically depressed instead of being tested for thyroid antibodies, and to think of the patients who start on thyroid hormones without consideration of dosage and form, resulting in ongoing symptoms, including depression.
The good news is that, once a diagnosis of Hashimoto’s (or thyroid disease) has been made, we can start looking for and addressing the root causes that might be leading to feelings of depression, including optimizing thyroid hormones. This article focuses on some of the low-hanging fruits that can help many people with depression feel better.
In this article, you’ll learn about:
- The connection between Hashimoto’s and depression
- Root causes of depression
- Strategies and solutions for depression that can help some 80 percent of people feel better
Depression and Hashimoto’s: What’s the Link?
Clinical depression, or major depression, is a mental health disorder characterized by persistently depressed mood or loss of interest in activities, causing significant impairment in daily life. Symptoms and severity can vary from person to person. It is estimated that some 21 million adults (8.4 percent) in the U.S. have experienced major depression at least once, and the prevalence is greatest in women and young adults. (1)
It might surprise you to discover that Hashimoto’s (and other thyroid disorders) and depression often co-occur — most people are unaware of how frequently this happens. A 2018 review paper found that “the chance of developing symptoms of depression that were of clinical relevance is 3.3 times higher among patients with hypothyroidism compared with healthy controls.” (2)
In Hashimoto’s, there is a breakdown of the thyroid gland, which can rush thyroid hormones into the bloodstream, resulting in transient hyperthyroidism. This can result in symptoms such as agitation, anxiety, and even psychosis. Anyone who has experienced symptoms of hyperthyroidism (due to the fluctuations in thyroid hormone often seen in Hashimoto’s) can describe how terrible this feels. (3)
Once the thyroid hormone is cleared out, the person may be functionally hypothyroid, which is linked with symptoms of depression, such as apathy, low mood, fatigue, and brain fog.
Thus, it’s possible that some cases of depression are related to the thyroid. (4) In fact, one reader with thyroid disease told me, “I feel like I’m sitting on the sidelines of life, watching everyone else enjoy their journey, wondering if I’ll ever have my zest for life back.”
If you are feeling alone and like no one believes you, please know that you are not alone, and it’s not in your head! I suggest reading this article about what it feels like to have Hashimoto’s to understand that many people struggle with feelings of depression and more, and it can take a while to get a proper diagnosis.
A study in 2004 found an association between the presence of a mood disorder, and the presence of thyroid peroxidase (TPO) antibodies. (5) Other research has connected depression, distress, obsessive-compulsive symptoms, and anxiety, with high levels of TPO antibodies. (2,6) TPO antibodies are early signs of an autoimmune attack on the thyroid, even when one’s TSH (thyroid stimulating hormone) number is still in a range that is considered normal.
In my experience, appropriate identification and treatment of a thyroid condition can resolve symptoms of depression. I’ve also seen plenty of instances where people have enjoyed well-deserved levels of health and happiness after addressing the underlying root causes and consequences of thyroid disease.
Conventional Treatments for Depression
Research supports the link between mood disorders and Hashimoto’s. For example, people with bipolar disorder (as well as depressive and anxiety disorders) were found to have a higher prevalence of antithyroid antibodies. (To further complicate the issue, prescription lithium, a medication often used for bipolar disorder, can actually trigger Hashimoto’s. However, nutritional lithium, which is an extremely low dose compared to prescription medication, may offer some mood benefits with lower risks. I encourage you to read more about that in the linked article.)
Doctors who are aware of the link between thyroid issues and mood disorders will take a deeper look at the role of thyroid disease and may consider thyroid medications in those presenting with symptoms. Likewise, progressive psychiatrists will test all of their patients who present with new-onset depression, anxiety, and mental health symptoms for thyroid disorders, and will often be open-minded about prescribing thyroid medication.
Unfortunately, despite all of the research that’s out there, these types of psychiatrists are a minority, and sometimes people are misdiagnosed (and even hospitalized) with conditions like bipolar disorder or schizophrenia when, in fact, they had thyroid imbalances.
In the majority of cases, conventional doctors favor the use of antidepressants (or a referral to a psychiatrist)! “Antidepressant” is a common name for the type of medication used to treat depression. (For a lot of people, Prozac comes to mind, though not all of the medications work on the same pathways as Prozac.)
That said, the most common antidepressants are SSRIs (selective serotonin reuptake inhibitors). These include brand names such as Zoloft, Prozac, Celexa, and Paxil. These drugs work by decreasing serotonin (our “happy hormone”) reuptake (reabsorption) in the brain, which leaves more serotonin available in the brain to positively affect mood. Common side effects of SSRIs include nausea, sexual dysfunction, insomnia, nervousness, and tremors.
Another commonly prescribed group of antidepressants is called SNRIs (serotonin and norepinephrine reuptake inhibitors). Cymbalta, Effexor XR, and Pristq all fall into this category of drugs that work by improving serotonin and norepinephrine (a neurotransmitter and hormone in the nervous system) levels in the brain. Common side effects include nausea, drowsiness, fatigue, constipation, and dry mouth.
Wellbutrin (bupropion) is another medication that has a few different indications. Most commonly, it’s used as an antidepressant that works on the norepinephrine and dopamine pathway and may be given as a stand-alone medication, or in combination with SSRIs to counteract the sexual side effects and fatigue caused by SSRIs. This medication is also FDA-approved for smoking cessation. (I’ve written about the connection between smoking and Hashimoto’s before, and I personally took bupropion in college for the purposes of smoking cessation.) This medication may also help with weight loss, focus, and energy. However, it can also lead to a suppression of TSH, the communication hormone that tells our body to make more thyroid hormone — potentially resulting in what is known as “central hypothyroidism,” where the TSH is normal but the actual thyroid hormones (T3 and T4) are low because the communication pathway isn’t working properly. (7,8)
I took this medication in college around the time I started having thyroid symptoms, and I remember that I felt more focused and energetic when I took it. I often wonder if this medication either masked some of my symptoms, contributed to my thyroid hormones being low, or potentially led to a suppression of TSH, masking the fact that I was hypothyroid whenever I was checked. This is why I often recommend doing a full thyroid panel to screen for thyroid conditions, and why depression is a big red flag for me when it comes to thyroid conditions.
Additionally, medications that were once traditionally used for treating schizophrenia are now used as “add-on” therapies for treatment-resistant depression. In the real world, as a consulting pharmacist, I saw a lot of heavy-duty use of these medications, and in some cases, this led to debilitating side effects (fainting, lethargy, loss of balance, sexual side effects, and metabolic syndrome, with some individuals earning over 100 pounds in the course of a year or two after initiating these medications).
Do Antidepressants Help with Depression?
When I hear people in natural medicine speaking about the evils of antidepressants, I think of my deceased loved one… oh, how I wish he had considered antidepressants, instead of taking his life. While it’s true that most mood-altering medications do have some unfavorable side effects, they can help some people feel better, and can save lives.
At the end of the day, as someone who wants to alleviate the world of suffering, I am supportive of most methods people use to heal.
As someone who has dispensed antidepressants, taken antidepressants, and monitored patients who were initiated on antidepressants, I can tell you firsthand that they do work really well for some people. I have had patients come to my pharmacy in deep despair, clutching onto their first prescription for an antidepressant — I sometimes would just listen to my patients for hours, on the phone in the late evenings when the pharmacy was quiet, and would see them feeling better and better every month they would come in to get their refills, often with a spark of hope in place of the dark shadow they carried at our first meeting.
That said, antidepressants don’t work for everyone. A major study completed in 2006, the STAR*D trial, showed that around 30 percent of people were “responders” to most antidepressants. Additionally, the STAR*D trial found that less than five percent of people were found to be in remission from depression with SSRI drugs, even after using them for a year. (9)
(Please note that if you are currently taking prescription antidepressants, it is important not to stop taking your medications without the oversight of your physician or therapist.)
Side Effects
Additionally, as I alluded to earlier, side effects are common with mood-altering drugs.
While I believe most medications have their time and place, the truth is, most mood-altering drugs are “dirty drugs” (this is official pharmacist lingo, lol). They interact with many receptors, leading to a long list of symptoms.
As a pharmacist, I often got reports from my patients and clients of feeling like zombies, gaining weight, having “dulled” feelings, living in a fog, having sexual dysfunction, becoming manic, and feeling worse on antidepressants and other mood-altering medications.
Suicidality
One of the scariest side effects of antidepressants that I learned about in pharmacy school is increased suicidality. We were taught that some people who were prescribed medications for depression could be more likely to die by suicide within weeks of starting them. The theory proposed to us students was that “people got more energy before their mood improved… and thus, this burst of energy gave them the opportunity to take their lives.”
Increased suicidality is a possible effect of antidepressants for a few reasons. For instance, it can happen if the drug is just not the right fit for the person, if a person is prescribed the wrong type or dose of medications, or if there are cofactors such as alcohol abuse present. It can’t always be predicted because different drugs work differently for each individual. That’s why, when these drugs are prescribed for the first time, a practitioner should carefully monitor the patient, and will often start with a lower dose, then increase it once no negative symptoms are reported.
In any case, this possibility of suicide was so scary to me as a young practicing pharmacist.
Suicide is a permanent solution for a temporary problem, and is devastating for loved ones of the deceased, who often go on to have post-traumatic stress disorder, survivor’s guilt, and even new onset autoimmune disease. (One day I’ll write more about my personal connection to loss… but for now, if you’re reading this and struggling with depression, I want you to know that you can feel better — and there are so many people and things that can help you. Don’t give up.)
Drug Dependence
Antidepressants can also cause a downregulation of our internal production of neurotransmitters. This means that people can become dependent on taking them and have withdrawal symptoms when they try to come off of them.
When I was a consulting pharmacist, I saw this firsthand, and have worked with monitoring numerous people to help them slowly wean off antidepressants.
This dependence occurs because antidepressants prevent us from properly clearing serotonin from our brains, causing it to stick around longer. Unfortunately, the body takes notice of all of this serotonin hanging around. Soon, we begin to produce less serotonin, and we become less sensitive to the serotonin we do have. When not addressed, this result may become permanent.
Beyond antidepressants, I’ve seen other mood-altering drugs being used for refractory depression (depression that doesn’t respond to medication treatment), some “off-label,” others with FDA approval.
For example, some of the “dirtiest” drugs out there include antipsychotic medications like Seroquel, Risperdal, and in particular Zyprexa. They have been traditionally used for schizophrenia, but are now being used for depression as well. I’ve seen people gain hundreds of pounds in the course of a year, become diabetic, lethargic, and withdrawn, and develop irreversible, involuntary movements and painful muscle contractions, from using antipsychotic medications.
From 2008 to 2011, the majority of my recommendations as a consultant pharmacist were to reduce or taper antipsychotic medications for clients due to the horrible side effects and lack of perceived benefit. From 2012 onwards, one of the key deliverables of my job was to help reduce the use of antipsychotic medications in the elderly.
Furthermore, I think it’s important to understand the root cause of the problem. For example, giving a person mood-stabilizing medications because of fluctuations in mood (due to Hashimoto’s), is like putting masking tape over the “check engine” light in a car, instead of checking the engine.
Antidepressants alone should never be the sole solution, even for a person with severe depression and anxiety. If you are someone who is taking antidepressants, root cause solutions can help you get the most benefit from them, and can even help you wean off of them (under your doctor’s supervision).
As a pharmacist, I really got a kick out of this article from the satirical news publication The Onion:

Let’s dive in and discuss some of the root causes of depression (including, but not limited to thyroid issues), as well as some solutions beyond medications.
The Root Cause Approach
I remember speaking to one of my young clients who was living in a mental health group home, about his goals, in my past job as a consultant pharmacist. He mentioned that he had hoped to be free of psychiatric medications, yet because of his diagnosis, I was so sad that our team of healthcare professionals would have to tell him that he would not meet his goal, and that he needed to choose a more “realistic” goal. In conventional medicine, medications are often life-long. Thankfully, I now know that psychiatric medications are not a life sentence.
The amazing thing that I’ve learned with functional medicine is that many people with lifelong psychiatric diagnoses can recover after receiving proper thyroid care. This is because many of the same root causes, triggers, and strategies that help Hashimoto’s, can also help depression (when the root cause of depression or a mood disorder is due to the thyroid). In fact, 81 percent of the participants in my Hashimoto’s Self-Management Program reported an improvement or resolution of depression!
One reader shared how liberating and transformational it was to realize the depression was related to their Hashimoto’s:
“One year ago, I was feeling anxious, depressed, and like I was going crazy! I was sent to a psychiatrist and prescribed Seroquel [an antipsychotic medication] and clonazepam [an anxiety medication]. 5 months later, I read your blog and went to my primary care doctor and demanded testing for Hashimoto’s. I wasn’t going crazy, I had TPO Antibodies well into the 600 range. I am being weaned off of the psychiatric meds and I immediately changed doctors. Thank you, Dr. Wentz, or I would still be spending thousands on a psychiatrist. And my TPO is slowly coming down.”
While there are many different root causes, strategies, and solutions for depression, I want to focus on a few low-hanging fruits that can help a person with depression, whether used in conjunction with antidepressants, or on their own. Many of these can be DIY options, as well as approached with the help of your primary care doctor.
These include:
- Optimizing thyroid hormones
- Making dietary changes
- Addressing nutrient deficiencies
- Utilizing supplements that have been shown to improve mood and stress
- Implementing mood-boosting lifestyle changes
Thyroid Hormone Optimization
First and foremost, If your TSH is elevated, you may need to consider thyroid hormone medications.
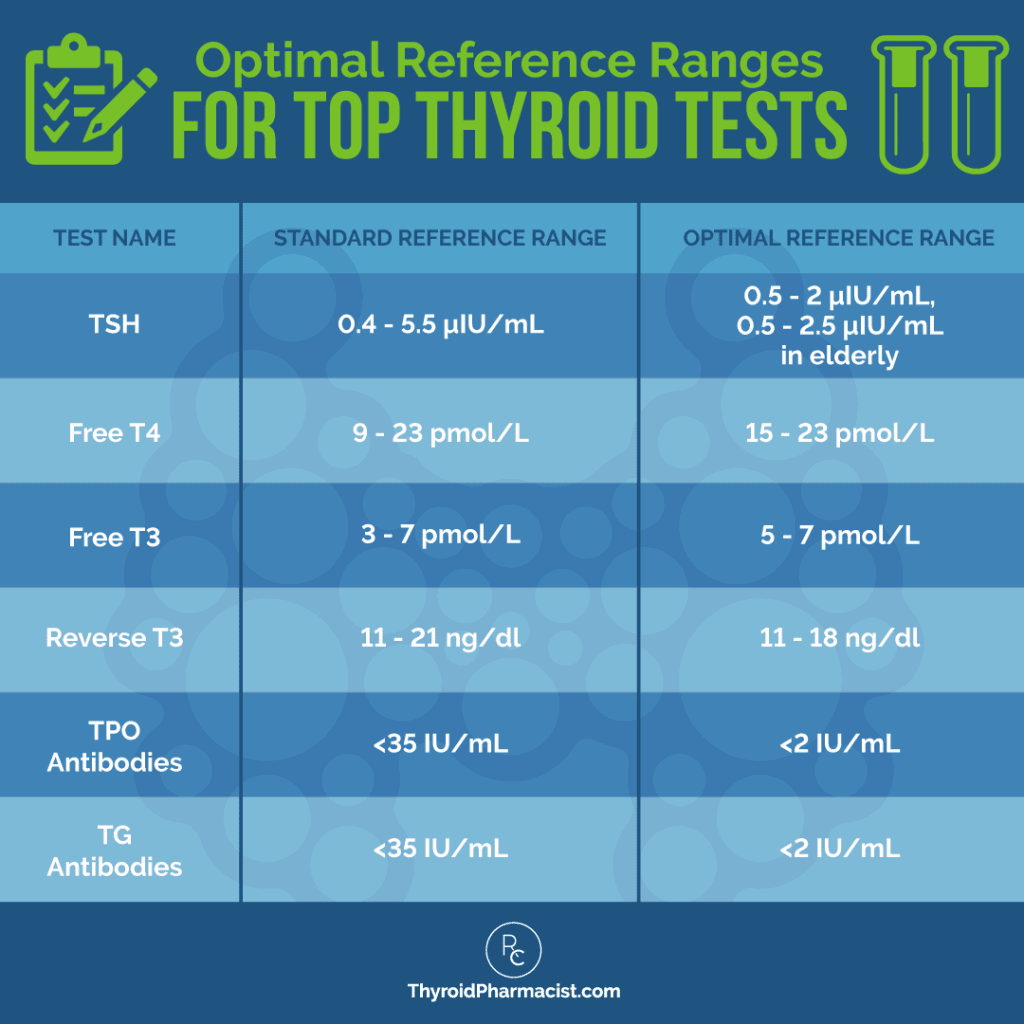
If you’re already on thyroid medications, you may need to adjust your current dosage to optimize your TSH levels. A survey of over 2000 Root Cause readers found that as far as medications and mood, getting TSH levels between 1 and 2 μIU/mL, and in some cases, under 1 μIU/mL, helped a person improve their mood symptoms. (Levels that are too high or too low indicate an imbalance of thyroid hormone levels and have been associated with various symptoms, including depression and anxiety.)
However, it’s important to note that some people continue to have these symptoms despite taking medications like Synthroid, levothyroxine, or Levoxyl. Not everyone can be optimized on a T4 medication alone.
One of the biggest signs that a person with thyroid disease is not converting T4 to the active T3 properly, is depression.
Additionally, medical studies have shown that 25 percent of people who do not see improvements with antidepressants, report feeling better once they were started on Cytomel® (a T3-containing thyroid hormone). (9)
If you are still having symptoms of depression while on your thyroid medications, consider talking to your doctor about switching your medications.
Taking a T3-containing medication, in particular, has been shown to reduce symptoms of depression. Around 60 percent of readers whom I surveyed, reported an improved mood after switching to a T3/T4 combo medication like Nature-Throid, WP Thyroid, Armour, or a compounded T4/T3 version.
You may want to read my articles on understanding your thyroid labs and taking thyroid medications for more information on how adjusting thyroid medication dosages or switching medications can help optimize your thyroid hormone levels and elevate your mood.
Dietary Changes
I have found that for some people with Hashimoto’s, their depression may in fact be a sensitivity reaction to food(s).
Some of the most common food sensitivities that can lead to symptoms of depression are gluten, dairy, grains, soy, nuts, and seeds. Eliminating these foods from one’s diet can bring enormous relief to a person’s mood and mental state. In fact, in my survey of readers with Hashimoto’s, 60 percent of people reported symptoms of improved mood by eliminating gluten, 59 percent saw improvements by going grain-free, and 45 percent by giving up dairy. I recommend starting with an elimination diet to begin to uncover the foods that are problematic for you.
Additionally, balancing blood sugar levels is one of the most important components in reducing anxiety for people with Hashimoto’s, and can have an impact on symptoms of depression as well. When insulin levels swing from high to low, it’s like being on an emotional rollercoaster that can cause some of the extreme emotions that are characteristic of mood disorders. Of the people with Hashimoto’s that I surveyed, 61 percent reported improved mood with a low glycemic index diet, while 65 percent experienced improvement on a sugar-free diet.
Nutrients for Depression
Addressing nutrient depletions can be a game changer when it comes to relieving depression. Oftentimes, a deficiency in a key nutrient results in many of the symptoms associated with depression, and supplementing with a quality supplement can make all the difference in improving mood.
Nutrient depletions that are often seen in people experiencing symptoms of depression include:
- Vitamin B6: Depression can be caused by something so simple as a deficiency in B6, and a recent study showed that high-dose vitamin B6 supplementation reduced anxiety and depression. (10) B6 is required for the production of neurotransmitters, and unlike antidepressants that artificially raise the levels of neurotransmitters, B6 has very few side effects. One clue that you may be deficient in B6 is poor dream recall. I generally recommend a dose of 50 to 100 mg. The pyridoxine form can also be used; however, doses above 300 mg should be avoided due to the potential of induced peripheral neuropathy. I’m excited to share that I’ve added P5P to the Rootcology portfolio, and that Pure Encapsulations also offers P5P. The P5P version of B6 can help to promote serotonin production, leading to a more positive mental outlook, better gut health, and an improved response to stress. (As a bonus, it can also help with gut health, blood sugar balance, and menstrual symptoms like water retention.)
- Vitamin B12: A deficiency in B vitamins, particularly B12, can have a huge impact on mental health. One study found that one quarter of women who were diagnosed with severe depression were deficient in this crucial nutrient. Of the readers with Hashimoto’s that I surveyed, 56 percent experienced an improved mood when they began supplementing with B12. (11,12)
- Methylfolate: Studies have shown that people with low levels of folate have a 7 percent response rate to treatment with antidepressants, while those with high levels of folate have a 44 percent response rate; therefore, it is often used in the treatment of depression. You can take methylfolate as a standalone supplement, or as part of a combination product like MTHFR Pathways. (13)
- Iron (ferritin): Several symptoms of iron deficiency are similar to that of depression: fatigue, irritability, and brain fog. I personally became iron deficient while pregnant, and felt like I became tearful and emotional overnight… These symptoms are usually considered “normal” for pregnant women, yet iron deficiency is the most common deficiency in pregnancy. I was already taking an oral iron supplement, but ended up needing to supplement with two burgers a day, and iron IVs, to stay happy. One day I told my husband that I didn’t feel loved because he hadn’t gotten burgers for me that day. 🙂 Testing iron and ferritin levels is incredibly important, and proper management may bring relief to symptoms of depression for many people. (As a side note, iron deficiency is more common in pregnant and menstruating women, while iron overload is more common in men and postmenopausal women. An overload of iron can also lead to mood alterations, so be sure to get tested and not just supplement.) (14,15)
- Omega-3: A number of studies show that omega-3 fatty acids can be effective against the treatment of major depressive disorder and other psychiatric disorders, with no associated side effects. I generally advise 1 to 4 grams per day for most people. (16)
- Vitamin D: Most people, especially those of us living further away from the equator, are deficient in vitamin D, and a deficiency in this important nutrient has been linked to elevated thyroid antibodies and depression. Sixty-four percent of my readers have reported improvements in mood when they’ve taken a D3 supplement. 5000 to 10000 IU per day is what it usually takes to get your vitamin D levels in range. I do recommend testing for vitamin D, and supplementing accordingly. (17)
- Magnesium: Multiple studies have linked magnesium deficiency with depression and anxiety, as this vital nutrient plays a key role in hormone balance and brain chemistry. Magnesium is required for the production of the sex hormones progesterone, estrogen, and testosterone, and also helps regulate cortisol — all of which impact mood and cognitive function. Magnesium is also an important component in thyroid hormone production, and helps balance blood sugar — key factors in mood stabilization. (18,19)
- Selenium: Selenium is essential for thyroid hormone synthesis. Research shows that it is also closely tied to mood disorders and cognitive function. Selenium deficiency is not only common in those with Hashimoto’s, but also with depression. (19,20) I often recommend Selenium from Pure Encapsulations, as it is generally well-tolerated.
- Myo-Inositol: Small studies have found that myo-inositol can help with depression as well as with obsessive-compulsive symptoms. It has also been shown to be a promising nutrient in reversing Hashimoto’s and normalizing TSH levels. (21, 22) I’ve seen success with Rootcology Myo-Inositol Powder in helping clients get a better sleep, balance hormones, and improve their mood.
Stress Response Support
In my experience, treating hypothyroidism without treating the adrenals, is one of the biggest reasons people continue to feel exhausted despite receiving treatment with thyroid hormones — and it can also lead to symptoms of depression.
The adrenal glands release hormones, such as cortisol and adrenaline, that impact many important functions throughout the body, including stress tolerance and mood. In cases of chronic stress, the never-ending presence of stressful, yet non-life-threatening situations, can lead to the constant activation of the stress response. To help meet the demand for cortisol, your body will decrease the production of other hormones normally produced by the adrenals, such as progesterone, DHEA, and testosterone. (23,24)
Eventually, with enough chronic stress, your body becomes overwhelmed and desensitized to the usual feedback loop, and stops sending messages to the adrenals to produce more hormones or less hormones, no matter what’s happening.
In the functional medicine community, we call this adrenal fatigue.
If you think stress could be at the root of your depression, you may want to look into supporting your adrenals. As a starting point, I recommend the “ABCs” — Adaptogens, B vitamins, and vitamin C.
Adaptogenic herbs support the body’s ability to deal with stressors and are thought to work by normalizing the hypothalamic-pituitary-adrenal (HPA) axis. Some herbs, such as ashwagandha, can help normalize thyroid hormone levels, as well as support the body’s stress response. (25,26)
Of the readers I surveyed, 77 percent said their mood improved when they took adaptogenic herbs.
The B vitamins and vitamin C become depleted during high cortisol production. In particular, deficiencies in pantothenic acid (B5) and biotin (another B vitamin) have been linked to decreased adrenal function in animals and humans. Meanwhile, vitamin C helps to regulate cortisol and prevent blood pressure from spiking in response to stressful situations. (27,28)
My Rootcology Adrenal Support supplement contains all three ABCs, but since it contains licorice root extract, I do not recommend it for those with high blood pressure. Pure Encapsulation’s Daily Stress Formula is a great option for supporting the adrenals of those who have high blood pressure.
Lifestyle Interventions
There are many types of therapies, exercises, and activities aimed at reducing depression — the important thing is finding one that will work for you. This may take some experimentation, but a few of my favorite forms of mental health therapy include:
- Bright light therapy: Bright light therapy (BLT) is considered among the first-line treatments for seasonal affective disorder (SAD), yet a growing body of literature supports its use in other mental health conditions, including non-seasonal depression. BLT uses a lamp to mimic sunlight to adjust the person’s circadian rhythm and elevate their mood. I’m a big proponent of being out in nature and enjoying the sunshine (especially on a beach vacation); however, those of us living in colder climates may not always have the ability to escape. In such cases, you can purchase a therapy light online to sit under for 15 minutes a day, in the comfort of your home.
- Meditation: Stress and anxiety are major triggers of depression, and meditation can alter your reaction to those feelings by training the brain to sustain focus, and return to that focus when negative thinking arises. Meditation has even been found to change certain regions of the brain that are linked with depression. There are many apps that can help you begin a meditation practice (Headspace is a popular one), but even just closing your eyes, sitting still, and focusing on your breath for five minutes is a wonderful place to start.
- Exercise: Research has shown that exercise works as well as antidepressants for some people with depression. (29) While high-intensity exercise releases the body’s feel-good chemicals called endorphins, low-intensity energy over a sustained period of time causes the release of proteins called neurotrophic (or growth) factors. These proteins cause nerve cells to grow and make new connections, which improves brain function and makes you feel better. My favorite forms of exercise to give me a mental boost are hiking, yoga, and walking with my little family. 🙂
- Art therapy: The healing power of art is emerging as an evidence-based therapeutic modality for depression.
One meta-review published in 2015 examined the impact of art therapy on depression, anxiety, trauma, distress, inability to cope, and low self-esteem. It concluded that patients receiving art therapy (using the process of creating artwork as a form of mental therapy) had significant improvements in 14 out of 15 randomized control trials. (30)
By immersing themselves in the art of creation, people with depression are often able to push back against the darkness inside their minds and find ways to express themselves when words fail. You don’t have to consider yourself an “artist” to explore this form of therapy — it’s all about the process of creation, not the final product. Many years ago, at the suggestion of a grief and trauma therapist, I painted this mandala to express my grief. I still remember what I tried to convey through it. The red colors symbolize the intense pain I felt, the faint yellow, my exhaustion from crying, and the orange colors are signs of confusion. The flower outlines my struggle to keep it together at the time. Yet, you can also see hope, transformation, and healing on the horizon (as depicted through the little sunbursts).

- Yoga: Gentle forms of yoga, such as Yin Yoga and Hatha Yoga, have been shown to calm the nervous system and relax the mind. Many controlled studies have found benefits from yoga for depression and its symptoms, such as difficulty concentrating and lack of energy. The combination of meditation and physical movement involved in yoga provide two important elements for relieving depression: meditation helps allow a person to clear their mind, while controlled, focused movements help strengthen the body-mind connection. (31)
- Sauna therapy: Saunas provide many benefits for Hashimoto’s, including stress relief and mood elevation (I like to recommend infrared saunas specifically, but any type of heat therapy can be helpful). The sympathetic nervous system and HPA-axis try to respond to compensate when the body is stressed by the rising body temperature. When a person is in the infrared sauna, their norepinephrine levels rise, but the body’s stress hormones epinephrine and cortisol do not. Growth hormone, beta-endorphins, and prolactin also increase. Beta-endorphins account for the reason a sauna session feels so pleasurable. The muscles also relax, allowing the body to release any tension and be free of stress. During this time, the body’s parasympathetic nervous system takes over, putting the body in a state of complete relaxation. (32,33)
In my 2015 survey of 2332 readers with Hashimoto’s, 74 percent of people reported that using a sauna boosted their overall mood. (Please note that sauna use may not be recommended in specific circumstances, or for those with certain medical conditions. You can learn more about infrared sauna contraindications in my article on saunas and Hashimoto’s.)
- Neurofeedback: This is a form of biofeedback therapy that uses real-time displays of brain activity to help self-regulate brain function. Research has shown its effectiveness for a variety of brain-related conditions, including depression. I like the Neuroptimal system and recommend finding a local neurofeedback practitioner in your area who has one.
- Eye Movement Desensitization and Reprocessing (EMDR) Therapy: In this form of therapy, the individual thinks about the painful memory, then follows a series of finger movements performed by the therapist, to help desensitize the negative feelings associated with the traumatic experience. If your depression results from events that occurred in your past, utilizing therapy may be the path to healing. EMDR, or Eye Movement Desensitization and Reprocessing, is a method used by psychotherapists to help people eliminate the lasting effects of traumatic events. This type of therapy was initially developed by Francine Shapiro, PhD, who noticed that certain eye movements reduced the intensity of her disturbing thoughts and made her less anxious during a walk in nature. She tested the method with trauma victims suffering from PTSD, and published her findings in 1989, establishing it as an evidence-based level treatment for trauma and post-traumatic stress disorder. (34)
I highly recommend working with a therapist who specializes in EMDR if you have encountered traumatic events in your past. I assure you, you can get past them.
In terms of helping me cope with the traumatic loss of my loved one, I worked with Dr. Allan Botkin, the creator of IADC, a version of EMDR targeted to the loss of loved ones. The therapy was life-changing, and I recommend it to anyone who has lost someone.
Other Strategies to Address Depression
Some 80 percent of the people with Hashimoto’s that I surveyed reported that alternative therapies such as acupuncture and massage therapy improved their mood.
- Speaking with a counselor or therapist is another important step toward mental health for many people. Sometimes, talking through the problem can be the best way to find the root cause — especially if past trauma is a factor.
- I encourage you to seek an integrative-minded practitioner who is trained in functional medicine.
- Low-dose (nutritional) lithium may be helpful, and unlike prescription lithium, is not harmful to the thyroid. (Read my article on nutritional lithium for more information.)
- You may also try using amino acids, orthomolecular medicine, and the Organic Acids Test to help you find additional targets for healing. The Organic Acids Test can identify hidden causes of depression and autoimmune issues, such as yeast and/or mold, elevations in Clostridia bacteria, and altered neurotransmitters. (35,36)
Though this is not a comprehensive list of all of the therapies available to treat depression, they are easy places to start if you are looking for alternatives or complements to prescription antidepressants.
Takeaway
About 80 percent of my clients with depression who have followed the above-mentioned recommendations, report that their symptoms improved.
As always, I encourage you to take control of your own health and advocate for your needs. If your symptoms, including depression and other mood-related symptoms, are possibly related to your thyroid, be sure to advocate for comprehensive lab testing and the right medications (being under- or overmedicated can contribute to inaccurate lab tests and thyroid symptoms).
Additionally, I encourage you to look into the Root Cause Approach to healing Hashimoto’s and utilize the interventions listed above, as well as in my Hashimoto’s Protocol book, to begin improving your health today!
I love interacting with my readers on social media, and I encourage you to join my Facebook, Instagram, TikTok, and Pinterest community pages to stay on top of thyroid health updates and meet others who are following similar health journeys. For recipes, a FREE Thyroid Diet start guide, and notifications about upcoming events, be sure to sign up for my email list!
References
- Major Depression. National Institute of Mental Health. Updated January 2022. Accessed September 25, 2022. https://www.nimh.nih.gov/health/statistics/major-depression
- Siegmann EM, Müller HHO, Luecke C, Philipsen A, Kornhuber J, Grömer TW. Association of Depression and Anxiety Disorders With Autoimmune Thyroiditis: A Systematic Review and Meta-analysis [published correction appears in JAMA Psychiatry. 2019 Jun 19;:]. JAMA Psychiatry. 2018;75(6):577-584. doi:10.1001/jamapsychiatry.2018.0190
- Symptoms: Overactive Thyroid (hyperthyroidism). National Health Service. Updated September 2019. Accessed October 2022. https://www.nhs.uk/conditions/overactive-thyroid-hyperthyroidism/symptoms/
- Hage MP, Azar ST. The Link between Thyroid Function and Depression. J Thyroid Res. 2012;2012:590648. doi:10.1155/2012/590648
- Carta MG, Loviselli A, Hardoy MC, et al. The link between thyroid autoimmunity (antithyroid peroxidase autoantibodies) with anxiety and mood disorders in the community: a field of interest for public health in the future. BMC Psychiatry. 2004;4:25. Published 2004 Aug 18. doi:10.1186/1471-244X-4-25
- Müssig K, Künle A, Säuberlich AL, et al. Thyroid peroxidase antibody positivity is associated with symptomatic distress in patients with Hashimoto’s thyroiditis. Brain Behav Immun. 2012;26(4):559-563. doi:10.1016/j.bbi.2012.01.006
- Haugen BR. Drugs that suppress TSH or cause central hypothyroidism. Best Pract Res Clin Endocrinol Metab. 2009;23(6):793-800. doi:10.1016/j.beem.2009.08.003
- Honkanen, Emma A. MD et al. Bupropion Causes Misdiagnosis in Brain Dopamine Transporter Imaging for Parkinsonism. Clinical Neuropharmacology. 2019; 42(5):181-183. doi: 10.1097/WNF.0000000000000359
- Gaynes BN, Warden D, Trivedi MH, Wisniewski SR, Fava M, Rush AJ. What did STAR*D teach us? Results from a large-scale, practical, clinical trial for patients with depression. Psychiatr Serv. 2009;60(11):1439-1445. doi:10.1176/ps.2009.60.11.1439
- Field DT, Cracknell RO, Eastwood JR, et al. High-dose Vitamin B6 supplementation reduces anxiety and strengthens visual surround suppression. Hum Psychopharmacol. 2022;37(6):e2852. doi:10.1002/hup.2852
- Syed EU, Wasay M, Awan S. Vitamin B12 supplementation in treating major depressive disorder: a randomized controlled trial. Open Neurol J. 2013;7:44-48. Published 2013 Nov 15. doi:10.2174/1874205X01307010044
- Laird E, O’Halloran AM, Molloy AM, et al. Low vitamin B12 but not folate is associated with incident depressive symptoms in community-dwelling older adults: a 4 year longitudinal study [published online ahead of print, 2021 Dec 13]. Br J Nutr. 2021;1-22. doi:10.1017/S0007114521004748
- Shelton RC, Sloan Manning J, Barrentine LW, Tipa EV. Assessing Effects of l-Methylfolate in Depression Management: Results of a Real-World Patient Experience Trial. Prim Care Companion CNS Disord. 2013;15(4):PCC.13m01520. doi:10.4088/PCC.13m01520
- Lee HS, Chao HH, Huang WT, Chen SC, Yang HY. Psychiatric disorders risk in patients with iron deficiency anemia and association with iron supplementation medications: a nationwide database analysis. BMC Psychiatry. 2020;20(1):216. Published 2020 May 11. doi:10.1186/s12888-020-02621-0
- Richardson AC, Heath AL, Haszard JJ, Polak MA, Houghton LA, Conner TS. Higher Body Iron Is Associated with Greater Depression Symptoms among Young Adult Men but not Women: Observational Data from the Daily Life Study. Nutrients. 2015;7(8):6055-6072. Published 2015 Jul 23. doi:10.3390/nu7085270
- Wani AL, Bhat SA, Ara A. Omega-3 fatty acids and the treatment of depression: a review of scientific evidence. Integr Med Res. 2015;4(3):132-141. doi:10.1016/j.imr.2015.07.003
- Penckofer S, Kouba J, Byrn M, Estwing Ferrans C. Vitamin D and depression: where is all the sunshine?. Issues Ment Health Nurs. 2010;31(6):385-393. doi:10.3109/01612840903437657
- Serefko A, Szopa A, Poleszak E. Magnesium and depression. Magnes Res. 2016;29(3):112-119. doi:10.1684/mrh.2016.0407
- Wang J, Um P, Dickerman BA, Liu J. Zinc, Magnesium, Selenium and Depression: A Review of the Evidence, Potential Mechanisms and Implications. Nutrients. 2018;10(5):584. Published 2018 May 9. doi:10.3390/nu10050584
- Benton D, Cook R. The impact of selenium supplementation on mood. Biological Psychiatry. 1991;29(11):1092-1098.
- Mukai T, Kishi T, Matsuda Y, Iwata N. A meta-analysis of inositol for depression and anxiety disorders. Hum Psychopharmacol. 2014;29(1):55-63. doi:10.1002/hup.2369
- Benvenga S, Nordio M, Laganà AS, Unfer V. The Role of Inositol in Thyroid Physiology and in Subclinical Hypothyroidism Management. Front Endocrinol (Lausanne). 2021;12:662582. Published 2021 May 10. doi:10.3389/fendo.2021.662582
- Ranabir S, Reetu K. Stress and hormones. Indian J Endocrinol Metab. 2011;15(1):18-22. doi:10.4103/2230-8210.77573
- Kozlowska K, Walker P, McLean L, Carrive P. Fear and the Defense Cascade: Clinical Implications and Management. Harv Rev Psychiatry. 2015;23(4):263-287. doi:10.1097/HRP.0000000000000065
- Esmaealzadeh N, Iranpanah A, Sarris J, Rahimi R. A literature review of the studies concerning selected plant-derived adaptogens and their general function in body with a focus on animal studies. Phytomedicine. 2022;105:154354. doi:10.1016/j.phymed.2022.154354
- Sharma AK, Basu I, Singh S. Efficacy and Safety of Ashwagandha Root Extract in Subclinical Hypothyroid Patients: A Double-Blind, Randomized Placebo-Controlled Trial. J Altern Complement Med. 2018;24(3):243-248. doi:10.1089/acm.2017.0183
- Camfield DA, Wetherell MA, Scholey AB, et al. The effects of multivitamin supplementation on diurnal cortisol secretion and perceived stress. Nutrients. 2013;5(11):4429-4450. Published 2013 Nov 11. doi:10.3390/nu5114429
- Brody S, Preut R, Schommer K, Schürmeyer TH. A randomized controlled trial of high dose ascorbic acid for reduction of blood pressure, cortisol, and subjective responses to psychological stress. Psychopharmacology (Berl). 2002;159(3):319-324. doi:10.1007/s00213-001-0929-6
-
Recchia F, Leung CK, Chin EC, et al. Comparative effectiveness of exercise, antidepressants and their combination in treating non-severe depression: a systematic review and network meta-analysis of randomised controlled trials. Br J Sports Med. 2022;56(23):1375-1380. doi:10.1136/bjsports-2022-105964
-
Uttley L, Scope A, Stevenson M, et al. Systematic review and economic modelling of the clinical effectiveness and cost-effectiveness of art therapy among people with non-psychotic mental health disorders. Health Technol Assess. 2015;19(18):1-vi. doi:10.3310/hta19180
- Jean M, Umair M, Muddaloor P, et al. The Effects of Yoga on Bipolar Disorder: A Systematic Review. Cureus. 2022;14(8):e27688. Published 2022 Aug 4. doi:10.7759/cureus.27688
- Smith SM, Vale WW. The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues Clin Neurosci. 2006;8(4):383-395. doi:10.31887/DCNS.2006.8.4/ssmith
- Hussain J, Cohen M. Clinical Effects of Regular Dry Sauna Bathing: A Systematic Review. Evid Based Complement Alternat Med. 2018;2018:1857413. Published 2018 Apr 24. doi:10.1155/2018/1857413
- Shapiro, F. Efficacy of the eye movement desensitization procedure in the treatment of traumatic memories. 1989. https://onlinelibrary.wiley.com/doi/abs/10.1002/jts.2490020207
- Potera C. Molding a link to depression. Environ Health Perspect. 2007;115(11):A536. doi:10.1289/ehp.115-a536a
- The Clinical Significance Of Organic Acids Testing To Mental Health – How Fungal, Bacterial, Mitochondrial, And Other Test Markers Influence The Brain. Great Plains Laboratory, LLC. April 19, 2018. Accessed November 6, 2022. https://www.greatplainslaboratory.com/articles-1/2018/4/19/the-clinical-significance-of-organic-acids-testing-to-mental-health-how-fungal-bacterial-mitochondrial-and-other-test-markers-influence-the-brain
- Hadtstein F, Vrolijk M. Vitamin B-6-Induced Neuropathy: Exploring the Mechanisms of Pyridoxine Toxicity. Adv Nutr. 2021;12(5):1911-1929. doi:10.1093/advances/nmab033
Note: Originally published in November 2020, this article has been updated and expanded for thoroughness and accuracy.


