by Gregg A. Masters, MPH and Fred Goldstein, MS*
In the still unfolding operating ‘new normal‘ wrought by the COVID-19 pandemic the path forward presents perhaps the career challenge of a lifetime to both seasoned and emerging U.S. healthcare leadership. No doubt, in health system c-suites across the nation the strategic question is and will likely remain for some time, how to best position admittedly complex enterprises to re-tool, optimize and align their mission in service of the communities in which they operate.
There are many economic challenges we face as a nation, let alone the unique headwinds and potential ‘opportunities‘ health system leaders must assess. Yet, much is on the line. Vetting strategic signals from noise around the pandemic in order to identify the key actionable steps with the greatest potential to deliver the outcomes essential to maintain successful operational portfolios is the strategic imperative laid before our healthcare leadership.
Likely included in top of mind issues to be vetted is the need to examine the role of legacy momentum driven, fee-for-service-fueled health system (and related JV or affiliated entity) business models. Who can fault health system leadership for maximizing revenues to generate the bottom-lines typically required to support a broad range and mix of both ‘profitable’ and ‘un-profitable’ service lines? Yet, habituating (vs. innovating) to the inertia of an aging tapestry of payment incentives may have inadvertently played a role in incentivizing the ‘myopia‘ of short term performance vs. the re-tooling required by an aspiring value based enterprise focused on long term viability.
For instance, we’ve known for quite some time that an estimated 30% of the aggregate national healthcare spend is of the ‘waste, fraud and abuse (over-treatment)‘ variety. Yet whatever the percentage of an average health system’s base revenue can be so attributed, the historical contribution may have meant the difference between insolvency and viability for many health systems. In a production incentivized $3.7+ trillion annual spend healthcare economy, critical healthcare infrastructure (both professional and institutional) may have unwittingly put themselves ‘at risk’ by focusing solely on the short-term revenue optimization.
COVID-19: A Healthcare ‘Black Swan’ Event?
Wikipedia summarizes Nassim Taleb‘s theory of black swan events as follows:
The black swan theory or theory of black swan events is a metaphor that describes an event that comes as a surprise, has a major effect, and is often inappropriately rationalized after the fact with the benefit of hindsight. The term is based on an ancient saying that presumed black swans did not exist – a saying that became reinterpreted to teach a different lesson after black swans were discovered in the wild.
Does the disruption to U.S. healthcare operators presented by the COVID-19 pandemic qualify as a black swan event, or, was this ‘surprise‘ a wholly predictable event in the cross hairs of U.S. healthcare leadership for at least the last 20 years? For instance, might some of those ‘risk averse’ health system executives be re-assessing their choice to pass on percent of premium or global or partial PMPM capitated offers? Clearly those health systems that chose to work with their physicians and scalably enter into risk based contracts are in a better position than those who chose to stay with the familiarity of fee-for-servies incentives even of the ‘value based’ variety
Bottom-Line?
Without considerable transitional support if not operating subsidies to weather the storm and engineer the operating efficiencies of a ‘population centric’ health system with a holistic (vs. current payor class segmented book of business driven) mission to serve the communities in which they operate, our production driven health system chassis is at risk and on balance largely ill equipped to survive the demands of a post COVID-19 environment.
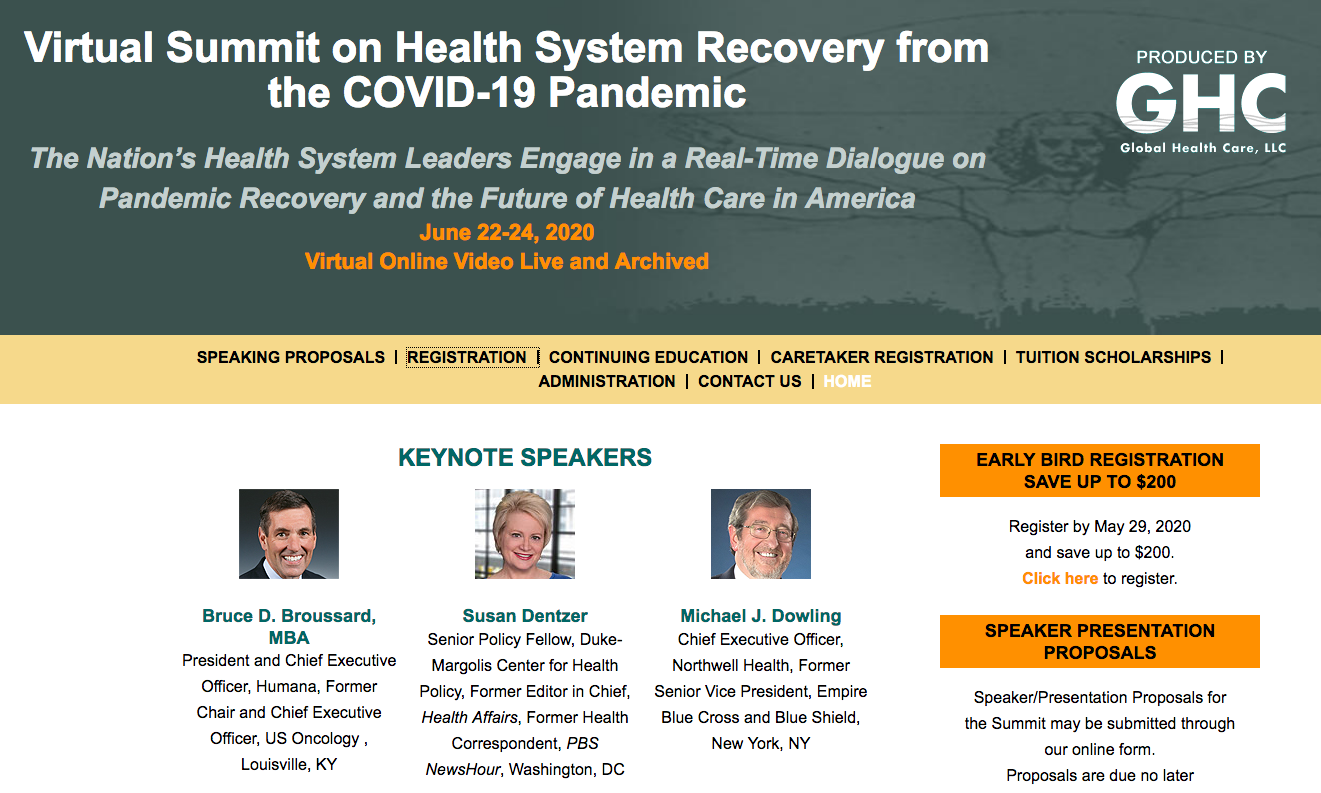
To address these critical issues and explore possible remedies, many national leaders will convene at the ‘ this June 22nd – 24th 2020. Loaded with top talent from major health systems, leading health plans and analysts this conference will explore the tremendous impact the COVID-19 Pandemic has had on the health care system and what the aftermath will look like.
Just thinking of the short and long term implications of the shutdown of elective procedures, the public health systems response, the management of the disease itself, the variable impact on communities around the country, the political response, lack of PPE, rapid move to telehealth, reopening facilites, employer responses and more, the effects have and will be profound.

Gaining an understanding of what the impact has been across the spectrum of healthcare delivery and finance and the likely road forward from key leaders who have and are managing through these issues will be critical to create a sustainable system able to deal with this new world.
This Virtual Conference will Bring together key leaders like:
- Michael Dowling, CEO of Northwell Health, whose facilites have been dealing with the largest outbreak of COVID-19 in the World in New York City,
- Humana’s CEO Bruce Broussard whose business has focused on the elderly on Medicare and innovative primary care models to
- Donald Rebhun, MD Regional Medical Director, HealthCare Partners Medical Group and Affiliated Physicians,
- Grace Emerson Terrell, MD, MMM, FACP, FACPE, General Internist, Wake Forest Health Network, chair of AMGA
- Susan Dentzer, Senior Policy Fellow, Duke-Margolis Center for Health Policy.
 And many others, this conference will provide a look into all sectors, players and issues. Here are just a few key highlights that caught our eye:
And many others, this conference will provide a look into all sectors, players and issues. Here are just a few key highlights that caught our eye:
Primary Care has been uniquely impacted, from the financial threats associated with closing/scaling back practices to the rapid uptake of virtual visits. Presentations in this area will include:
- The “New Normal”: How Primary Care can Reboot and Reopen
- Advanced Primary Care/Medical Home COVID Impact Update
- Health Care Without Walls: Telehealth and Virtual Care in the Public Health Emergency and Beyond
What about the move to value based care and alternative payment models? Are there opportunities in there, are some of these models a hindrance? Again some key presentations:
- ACO COVID Impact Update
- Bundled Payment COVID Impact Update
- MACRA COVID Impact Update
- Advanced Primary Care/Medical Home COVID Impact Update
And what of those areas that seem to receive less focus like The Post-Acute and Long-Term Care Systems in Covid-19 or Pandemic Palliative and Hospice Care. This conference will cover it all from an Update on Molecular and Serology Testing to Social Determinants of Health, Safety Net Hospitals and FQHCs to Big Data and AI. So join this two day conference to learn from others in your field and the broader healthcare system and help us all work to recover from this pandemic.
For a complete faculty listing and agenda, .
==##==
*Post sponsored by Health Care LLC.